본문
Factors Affecting Mealtime Difficulties in Older Adults with Dementia Living in Long-Term Care Facilities: A Multilevel Model Analysis

by Prof. Dukyoo Jung
Division of Nursing
PURE Research Profile
dyjung@ewha.ac.kr
Older adults with dementia frequently face challenges with eating, leading to issues like reduced nutrition, weight loss, and increased health risks. These mealtime difficulties are influenced by a variety of factors, including the cognitive and physical capabilities of the individuals, the knowledge, attitudes, and practices of direct care workers, and the characteristics of their living environment. This complex issue is best understood through the Social Ecological Model (SEM) which considers individual, caregiver, and environmental factors. This research employs a multilevel model analysis that not only takes into account individual characteristics such as cognitive impairment and functional ability but also integrates group-level factors like staffing levels and the care environment. This comprehensive approach is crucial for understanding the complex dynamics that contribute to mealtime difficulties.
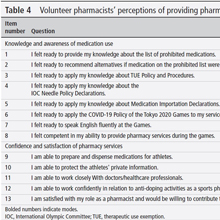
This study used a cross-sectional design and a multilevel model analysis based on the SEM to examine mealtime difficulties in older adults with dementia living in long-term care facilities. The study was quota sampling was performed based on region, institution grade, and the number of beds. Participants in this study included 342 dyads from 57 long-term care facilities, 114 direct care workers, and 342 older adults with dementia. Statistical analyses were conducted using SPSS 25.0, Excel, and MPlus 8.0, employing a three-level random intercept model for analyzing influencing factors.
In this study, the most significant impact on mealtime difficulties in older adults with dementia was found to be intrapersonal factors. These include gender, cognitive function, and the ability to perform activities of daily living (ADL). Specifically, those with diminished cognitive function and physical abilities encountered more difficulty in eating. This is often due to a decline in the ability to express their intentions and the challenges in using eating utensils, which are exacerbated by the progression of dementia. Therefore, caregivers in long-term care facilities require comprehensive training to adeptly identify and manage the varied mealtime difficulties in older adults with dementia, ensuring their support is specifically tailored to each resident's unique functional needs. This study also suggests that gender may influence these difficulties, but further research is needed due to inconsistent findings in previous studies.
Also, environmental factors such as meal assistant education, facility size, and the adequacy of dining environments were found to influence mealtime difficulties in older adults with dementia. Notably, mealtime difficulties were more prevalent in facilities where care workers had received training, which was an unexpected outcome. This paradox might be explained by the fact that 47.4% of these trained care workers scored below 50% in feeding knowledge tests, indicating that despite receiving training, their knowledge did not improve, and consequently, direct care workers may rely more on habit or experience than on formal education. However, previous studies have shown the importance of care workers' knowledge and attitudes in affecting mealtime difficulties. Therefore, this underscores the crucial need for continuous and effective education for care workers to enhance care quality and reduce mealtime challenges.
Furthermore, larger facilities faced greater mealtime challenges, likely due to a higher number of residents with reduced ADL and increased nursing demands. Previous studies suggest that higher nursing demand necessitates more direct care workers, emphasizing the importance of proper staffing to provide adequate assistance to older adults with significant nursing needs and mealtime difficulties due to low ADL.
Additionally, the study highlights the importance of creating a suitable mealtime environment. Current evaluations of Korean long-term care facilities primarily focus on the general environment and fall prevention, lacking specific guidelines for dining environments tailored to the needs of dementia patients. Therefore, developing comprehensive guidelines that address the unique dining needs of residents with dementia is crucial to minimize mealtime difficulties.
Lastly, at interpersonal factor, no variable was found that influenced mealtime difficulties. This is because the knowledge and attributes of the direct care workers who participated were distributed with low variance in the low score range. Therefore, to confirm the effect of interpersonal factor on meal difficulties, direct care workers must be analyzed again after improving their knowledge and attitudes to some extent through continuing qualitative meal difficulty education.
This study demonstrates how intrapersonal, interpersonal, and environmental factors collectively impact eating difficulties in older adults with dementia, underscoring the significant influence of intrapersonal elements and the necessity for a modifiable environmental approach in long-term care facilities.
* Related Article
Jung, D., De Gagne, J. C., Lee, H., Yoo, L., Park, J., & Choi, E., Factors Affecting Mealtime Difficulties in Older Adults with Dementia Living in Long-Term Care Facilities: A Multilevel Model Analysis, Journal of Nursing Management, Volume 2023, 8 pages, March 2023