본문
Effects of bone incorporation after arthroscopic stabilization surgeryfor bony Bankart lesion based on preoperative glenoid defect size
By Prof. Sang-Jin Shin (sjshin622@ewha.ac.kr)
Department of Orthopaedic Surgery, College of Medicine
Background: Recurrent shoulder instability after arthroscopic Bankart repair occurs more frequently over 20% glenoid bone loss, however, for lesions less than 20%, we have no scientific guidance what size of bone fragments may affect shoulder functional restoration after bone incorporation procedures. Union of bony Bankart fragments and restoration of glenoid anatomy are thought to be important for the glenohumeral stability, therefore, surgeons attempt to incorporate bone fragments regardless of size. Although instability has been shown over 20% glenoid bone loss; however, for lesions less than 20%, we have no scientific guidance what size of bone fragments may affect shoulder functional restoration after arthroscopic Bankart repair with bone incorporation procedures.
Purpose/Hypothesis: The purpose of this study was to analyze how preoperative glenoid bone defect size and bone fragment incorporation alter postoperative clinical outcomes by comparing the functional outcomes of shoulders with and without bony Bankart lesion. We hypothesized that there would be differences in postoperative clinical outcomes between the patients with and without bony fragments only in patients with a larger glenoid defect.
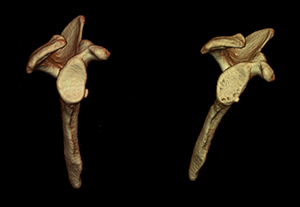
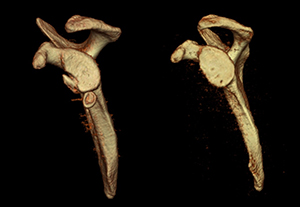
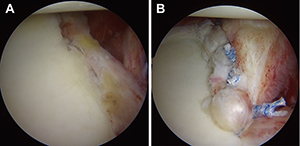
Methods: A total of 223 patients who underwent arthroscopic stabilization surgery for recurrent anterior shoulder instability were divided into two groups based on the presence or absence of anterior glenoid bone fragments. In each group, postoperative shoulder functional outcomes, sports activity level and recurrence rates were evaluated according to preoperative glenoid defect size (small: less than 10% (Fig 1); medium: 10–15% (Fig 2) and 15–20% (Fig 3); large: greater than 20% (Fig 4)). Arthroscopic single-row fixation was performed for patient with a Bankart lesion without bone fragment (Fig 5) and double-row fixation for patient with a bony Bankart lesion (Fig 6).
| Fig1 | Fig2 |
 |
 |
| Fig3 | Fig4 |
 |
 |
| Fig5 | Fig6 |
 |
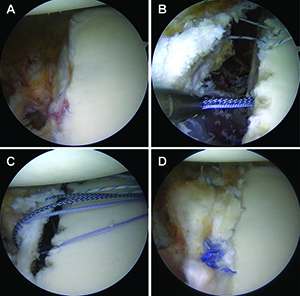 |
Results: In patients with glenoid defect less than or equal to medium size, there were no significant differences in postoperative clinical outcomes and sports activity levels between the two groups. However, in patients with large defect, those with bone fragments (ASES score: 92.3±2.7; Rowe score: 90.9±5.4) showed significantly superior clinical outcomes to those of patients without fragments (ASES score: 87.3±6.2, P=0.02; Rowe score: 84.8±7.3, P=0.04). (Table 1)
Table 1. Final clinical outcomes after arthroscopic stabilization procedure according to preoperative glenoid defect size.
| Preoperative glenoid defect size |
ASES score | Rowe score | ||||
| Group I | Group II | P value | Group I | Group II | P value | |
| < 10% | 94.3 ± 7.7 | 96.7 ± 5.4 | 0.37 | 94.5 ± 5.1 | 91.8 ± 7.3 | 0.09 |
| 10 - 15% | 93.3 ± 4.4 | 89.8 ± 13.8 | 0.99 | 93.3 ± 4.3 | 89.5 ± 13.1 | 0.07 |
| 15 - 20% | 91.8 ± 11.8 | 87.8 ± 15.6 | 0.46 | 91.9 ± 11.3 | 86.6 ± 16.1 | 0.17 |
| > 20% | 92.3 ± 2.7 | 87.3 ± 6.2 | 0.02* | 90.9 ± 5.4 | 84.8 ± 7.3 | 0.04* |
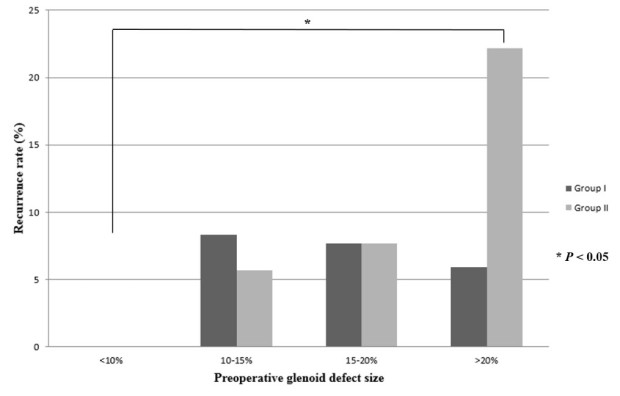
Among patients without bone fragments, recurrence increased significantly with increasing preoperative glenoid defect size (recurrence rates: 0% in small defect; 22.2% in large defect, P=0.01), whereas patients with bone fragments showed no increasing or decreasing tendency (Fig 7).
There were no significant differences in the final glenoid defect size, despite the wide range of preoperative and planned glenoid defect sizes, because of the different bone fragment resorption rates (Table 2).
Table 2. Postoperative changes in the glenoid rim morphologic characteristics of patients with bony Bankart lesions by glenoid defect size.
| Preoperative glenoid defect size | Fragment size (a) | Planned glenoid defect size (b) | Final glenoid defect size (c) | Resorption rate (d) | |
| Range | Mean | ||||
| < 10% | 4.6 ± 2.6 | 3.0 ± 2.7 | 1.6 ± 2.2 | 3.5 ± 2.3 | 63.3%*†‡ |
| 10 - 15% | 12.9 ± 1.6 | 11.4 ± 5.5 | 1.5 ± 1.7 | 4.8 ± 5.1 | 28.9% |
| 15 - 20% | 18.0 ± 1.7 | 11.4 ± 5.5 | 6.6 ± 2.9 | 9.0 ± 4.8 | 21.1% |
| > 20% | 28.7 ± 6.1 | 23.2 ± 7.9 | 5.5 ± 3.7 | 7.0 ± 5.1 | 6.5% |
All values are reported as percentages.
Resorption rate, d = (c – b) / a x 100%
* No significant difference compared to patients with preoperative glenoid defect size 10 - 15% (P = 0.22).
† No significant difference compared to patients with preoperative glenoid defect size 15 - 20% (P = 0.08).
‡ Significantly difference compared to patients with preoperative glenoid defect size greater than 20% (P = 0.02).
Bone fragment resorption was significantly higher in patients with preoperative glenoid defect size less than 10% than in patients with defects greater than 20%. Based on preoperative bone fragment size, the bone fragment resorption rate decreased with increased bone fragment size. Fragments less than 5% of the glenoid width showed significantly more resorption than fragments greater than 5% (Table 3).
Table 3. Postoperative bone fragment resorption rates by preoperative bone fragment size.
| Preoperative fragment size | Preoperative glenoid defect size | Resorption rate | |
| Range | Mean | ||
| < 5% | 2.0 ± 1.0 | 5.3 ± 4.8 | 72.8%*†‡ |
| 5 - 10% | 8.3 ± 1.3 | 16.4 ± 4.7 | 20.4% |
| 10 - 15% | 13.3 ± 3.0 | 19.2 ± 6.1 | 22.3% |
| > 15% | 23.1 ± 5.5 | 27.0 ± 5.1 | 10.8% |
All values are reported as percentages.
* Significantly difference compared to patients with preoperative fragment size 5 - 10% (P = 0.03).
† Significantly difference compared to patients with preoperative fragment size 10 - 15% (P = 0.02).
Conclusion: In the treatment of bony Bankart lesion, the effect of bone fragment incorporation was different according to preoperative glenoid defect size. In patients with preoperative glenoid defects less than 20% of the glenoid width, bone fragments incorporation after arthroscopic bony Bankart repair does not alter clinical outcomes, sports activity levels or recurrence rates, whereas in patients with defect greater than 20% of glenoid width, bone fragments incorporation improved clinical outcomes and recurrence rates.
* Related Article
Park I, Lee JH, Hyun HS, Oh MJ, Shin SJ, Effects of bone incorporation after arthroscopic stabilization surgery for bony Bankart lesion based on preoperative glenoid defect size, American Journal of Sports Medicine 46(9): 2177-2184, 2018